Definitions
Soft tissue rheumatism: Is the aggregate of clinical problems related to tendons, ligaments, fascia and bursae. They often present as a regional problem. They are quite common and compose 25% of a rheumatology practice.
Regional rheumatic disorders: Brings together all problems that present with localized pain. In addition to tendons, ligaments, fascia and bursae, it includes arthritis, bone disease. (ex., osteomyelitis), neurological problems (ex, carpal tunnel syndrome) and referred pain (ex., apical tumor of the lung ® shoulder).
Bursitis: Describes inflammation of a closed sac lined with synovial cells and having small amounts of synovial fluid within. They are present in areas of friction, facilitating movement of tendons and muscles and protect bony prominences from repetitive trauma.
Tendinitis: Describes inflammation of the tendon itself or the sheath that sometime surrounds it (tenosynovitis).
Bursitis
According to anatomists there are over 200 bursae in the human body. Many are inconstant or clinically insignificant. Some are generated by trauma in unusual places. Of those clinically significant (30 or so), we will discuss only five.
Important Bursae
(a) Subacromial bursa/Subdeltoid bursa- Located between the acromion and the rotator cuff (Figure 1). The subdeltoid bursa can be a separate bursa under the deltoid muscle or an extension of the subacromial bursa. Because of the great mobility of the shoulder joint, this area is subject to much movement and consequent irritation. It is the most common cause of shoulder pain. Since the bursae are often located next to the tendons, the term tendinitis and bursitis are often interchangeable because of the clinical difficulty in distinguishing these entities (ex., subacromial bursitis, supraspinatus tendinitis, rotator cuff syndrome)
b) Olecranon bursa- lies over the olecrannon process and the inflammation of this bursa is also known as “students elbow.”
c) Trochanteric bursa- lies between the hip capsule and the iliopsoas muscle and tendon (Figure 2). It is the most common cause of lateral hip pain.
d) Prepatellar bursa- located between the skin and the patella. Also known in the past as “housemaid knee.”
e) Achilles bursa- located between the calcaneus and the Achilles tendon. Not to be confused with a traumatic bursa created by ill-fitting shoes that appears between the skin and the Achilles tendon.
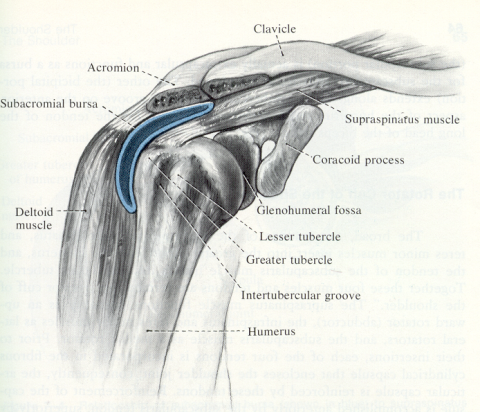
Fig. 1 Subacromial bursa
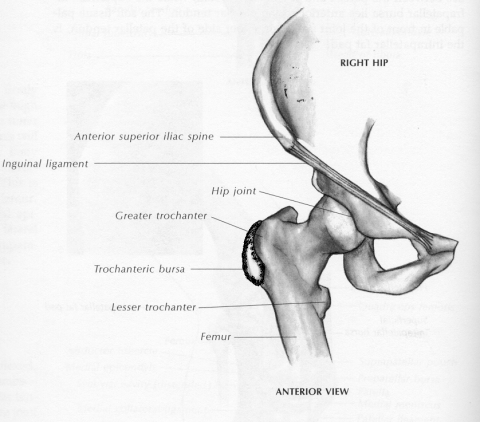
Fig. 2 Greater trochanteric bursa
Etiology
a) Trauma: acute or chronic
b) Overuse: leads to microtrauma
c) Systemic disease: tendon sheaths and bursae have the same cellular characteristics as synovium so are vulnerable to the same inflammatory processes (inflammatory arthritis, gout)
d) Septic: direct involvement from local injury or as part of a septic process
Diagnosis
a) Localized pain
b) Swelling: (only certain sites, ex., olecranon)
c) Erythema: Many times not apparent
d) Tenderness to palpation
e) Pain on specific maneuvers for the shoulder:
- Impingement sign- Abduction of the arm above 90 degrees produces pain in the shoulder. It suggests an inflamed subacromial bursa (Figure 3).
- Drop arm test- Slow lowering of the arm from full abduction leads to weakness and the dropping of the arm when below 90 degrees. Sometimes a slight tap is necessary. It suggests a complete tear of the rotator cuff (Figure 4).
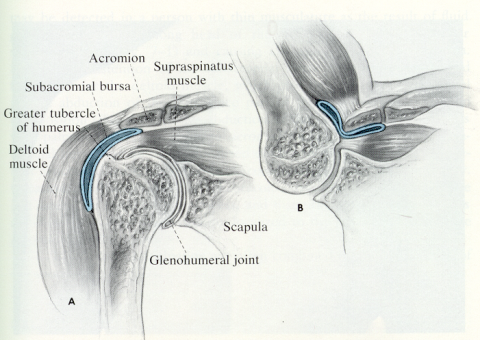
Fig. 3 Impingement sign.
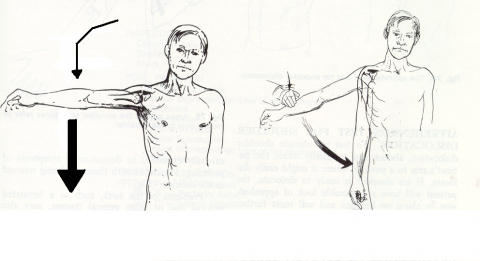
Fig. 4 Drop arm test.
Imaging Studies
X-rays of the region may reveal calcific deposits which are the result of previous inflammatory episodes. Other imaging techniques, such as ultrasonography and MRI can be very helpful. The latter technique is very sensitive in detecting edema.
Treatment
a) Rest: discontinue aggravating activities, immobilization for 7-10 days
b) Cold compresses: for acutely inflamed areas
c) Analgesic medication: acetaminophen
d) Anti-inflammatory medication: NSAIDs, corticosteroids
e) Aspiration and corticosteroid injection of inflamed bursa
f) Surgery: failure of conservative management a septic
Tendinitis
Pathogenesis
a) Intratendinous lesions- Occurs later in life and is primarily due to decreasing perfusion of the tendon associated with microtrauma. During attempts at repair, calcium salts can be deposited which appear on x-ray. It is then called calcific tendinitis. Commonly involved tendons include the supraspinatus and gluteus medius/minor. Tennis elbow, pain at the tendinous insertion located in the lateral epicondyle, is also considered a tendinitis.
b) Peritendinous inflammation or tenosynovitis- tendon sheaths in areas of increased friction are susceptible to inflammation and pain. De Quervain disease is inflammation of the tendon sheaths over the distal radial head (Figure 5) and "trigger finger" is the result of inflammatory thickening of the fibrous sheath (pulley) with fusiform swelling of corresponding flexor tendons (Figure 6). Sometimes the origin of the tenosynovitis can be septic either by direct penetration or by hematogenous spread.
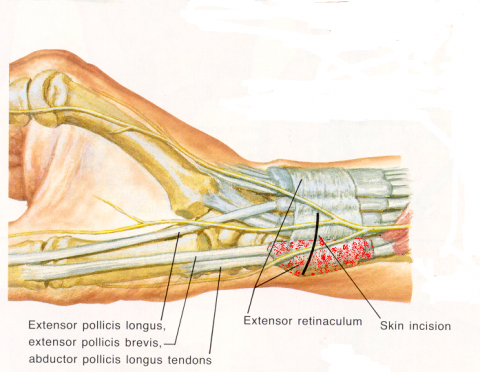
Fig. 5 De Quervain tenosynovitis
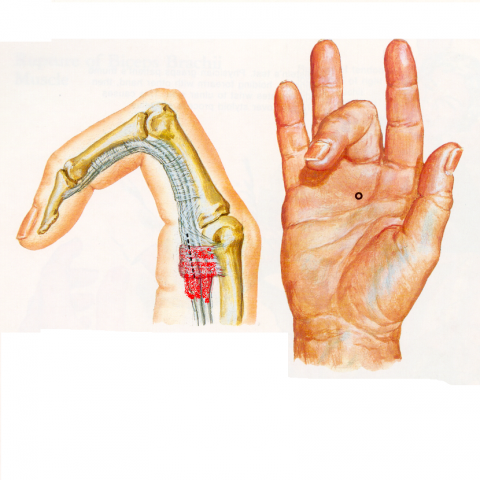
Fig. 6 Trigger finger
Diagnosis
Pain on motion is frequent. In de Quervain’s tenosynovitis stretching of the tendons is particularly sensitive and is called Finkelstein's maneuver (Figure 7). One may note overlaying warmth, swelling and tenderness, and, occasionally, erythema. Since tendons cross joints, distinguishing acute inflammatory arthritis from tenosynovitis can be difficult.

Fig. 7 Finkelstein’s maneuver
Treatment
a) Immobilization with splints or casts, slings or crutches
b) Physical therapy to avoid permanent stiffness
c) Local heat for pain relief
d) Analgesic medications
e) Anti-inflammatory medications (NSAIDs, systemic corticosteroids)
f) Local injection of corticosteroids and anesthetic combination
g) Surgery as a last resort
Carpal Tunnel Syndrome
Pathogenesis
Compression of the median nerve at the level of the wrist (Figure 8). It may be primary (idiopathic) or secondary to certain activities (typing, knitting, thumb rolling and kneading). It can be associated with systemic medical conditions ( inflammatory arthritis, pregnancy, gout, diabetes mellitus, hypothyroidism, amyloidosis and local tumors among others).
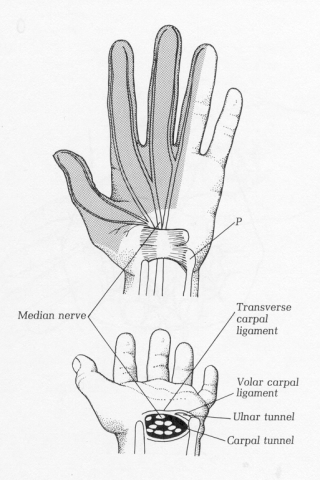
Fig. 8 Sensory distribution of the median nerve and its location in the carpal tunnel
Diagnosis
a) Early morning stiffness
b) Tingling or burning in the distribution of the median nerve
c) Sensory loss in median nerve distribution
d) Loss of fine motor function
e) Special tests:
- Tinel's sign- percussion of a nerve, in this case the median nerve at the ventral aspect of the wrist which produces pain and paresthesias along the median nerve distribution.
- Phalen's sign- Prolonged hyperflexion (up to 60 seconds) of the hands results in compression of the median nerve and similar complaints.
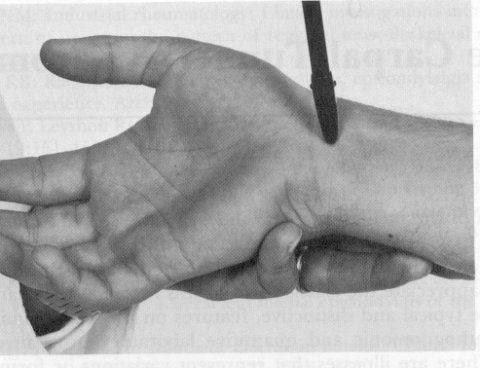
Fig. 9 Tinel’s sign
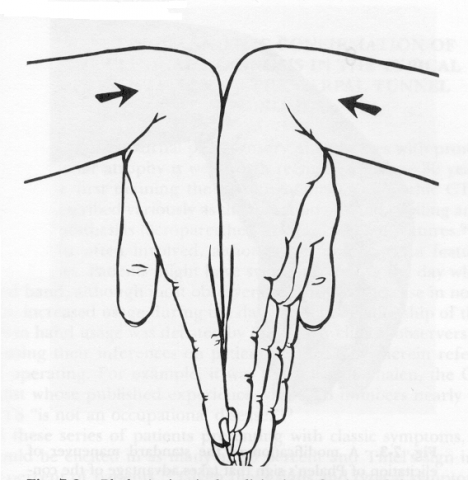
Fig. 10 Phalen’s sign
Ancillary Studies
a) Nerve conduction studies (NCV) can demonstrate a delay in sensory latency of the median nerve at the level of the wrist and helps exclude conduction abnormalities at other levels (ex., cervical spine).
b) MRI can show a deformed median nerve confirming the presence of compression.
Management
a) Immobilization may decrease inflammation and, therefore, symptoms.
b) Anti-inflammatory medications may diminish inflammation.
c) Local injection of corticosteroids and anesthetic
d) Surgical release of the transverse carpal ligament.
POPLITEAL CYST
Posterior extension of the synovial membranes into the popliteal area because of persistent fluid production in the knee. Most commonly seen with osteoarthritis and rheumatoid arthritis. Its rupture can produce sudden pain and swelling mimicking acute thrombophlebitis.
Diagnosis
Popliteal discomfort/pain, bulging of the popliteal region (noticeable on inspection when standing) and swelling (with ecchymosis) to the ankle/foot when it ruptures.
Imaging studies
Ultrasound, MRI. In the old days, arthrogram.
Management
Rest, steroid injection, rarely, surgery. R/O DVT in cases of suspected rupture. REFLEX SYMPATHETIC DYSTROPHY (Sudeck's atrophy)
Pathogenesis
Unknown but autonomic deregulation is evident.
Three stages:
1) hyperesthesia, hyperalgesia, altered color and temperature, edema and erythema;
2) further edema, thickening of skin, pigmentary changes and muscle wasting;
3) limitation of movement, contractures of the digits, atrophic skin changes and brittle, ridged nails.
Usually in an upper extremity. In children, a lower extremity is more likely. Often follow certain events-Soft tissue injury (40%), fractures (25%), postoperatively (20%), MI (12%), CVA (3%).
Clinical manifestations
Throbbing, burning pain, sensitivity to touch or cold , temperature and color alterations.
Diagnosis
Xrays( unilateral osteopenia), bone scan (increased uptake of affected limb because of increased bone turnover)
Management
In the following sequence: steroid injection (shoulder- if concurrent "frozen shoulder" is present) , vigorous physical therapy, sympathetic nerve blocks, systemic steroids, sympathectomy
Tarsal Tunnel Syndrome
Compression of the posterior tibial nerve at the level of the medial malleolus with paresthesias and pain extending along the plantar aspect of the foot to the toes. A positive Tinel sign can be found. Management is similar to that of the carpal tunnel syndrome.
Plantar Fasciitis
Is characterized by tenderness along the plantar aponeurosis particularly at its insertion to the calcaneus. Pain occurs on weight-bearing and can be elicited by percussion of the heel. Radiologically, one may see ossification of the insertion site (heel spur). Management includes re-distributing the weight peripherally away from the insertion site (“heel donut” does this very well), NSAIDs, and occasionally, local injection of corticosteroids and anesthetic, and rarely surgery.
SOFT TISSUE RHEUMATISM Rafael Grau, MD Suggested Reading: Primer of Rheumatic Diseases, 12th edition, Chapter 8, pp. 174-187, pp. 201-208.
Preparation:
After completion of the reading assignment, be prepared to:
- Name the most common sites for bursitis and tendinitis
- Identify the most common nerve entrapment syndromes
- Distinguish nerve entrapments from bursitis and tendonitis
Objectives:
Upon completion of the lecture, be able to:
- Explain the pathogenesis of soft tissue rheumatism
- Describe the tests used in the diagnosis of these conditions
- Discuss the medical management of these conditions

