Risk of Incident Knee Osteoarthritis and Clinical Outcomes Based on Imaging Biomarkers
Osteoarthritis (OA), a type of arthritis exemplified by deterioration of protective cartilage at the ends of bones, is the most common form of arthritis in the knee. Joint pain may worsen as cartilage gradually erodes over time. Most often, this degenerative “wear-and-tear” disease affects people age 50 or older, but it can occur at younger ages. It’s estimated to afflict 27 million people in the United States alone. Medicine, physical therapy and surgery can help alieve pain and maintain joint movement. The goal of the line of research in this project—which builds on prior work of the investigators and two other ongoing studies—is to identify key risk factors for development of radiographic knee osteoarthrtitis (ROA) and OA structural disease progression, and to identify potential targets for preventative and/or therapeutic interventions.
Addressing Ethnic/Racial Differences in Osteoarthritis Treatment
Osteoarthritis (OA) is the most common form of arthritis and is a leading cause of pain and disability among the elderly. Ethnic and racial differences in the outcomes of OA patients exist with Hispanics & African Americans more likely to experience pain from OA and less likely to be using effective OA treatments than non-Hispanic whites. The current project proposes to identify contributors to ethnic/racial differences in use of various OA therapies and to develop an educational tool to improve understanding and use of these treatments.
Biomechanical Treatment of Carpal Tunnel Syndrome
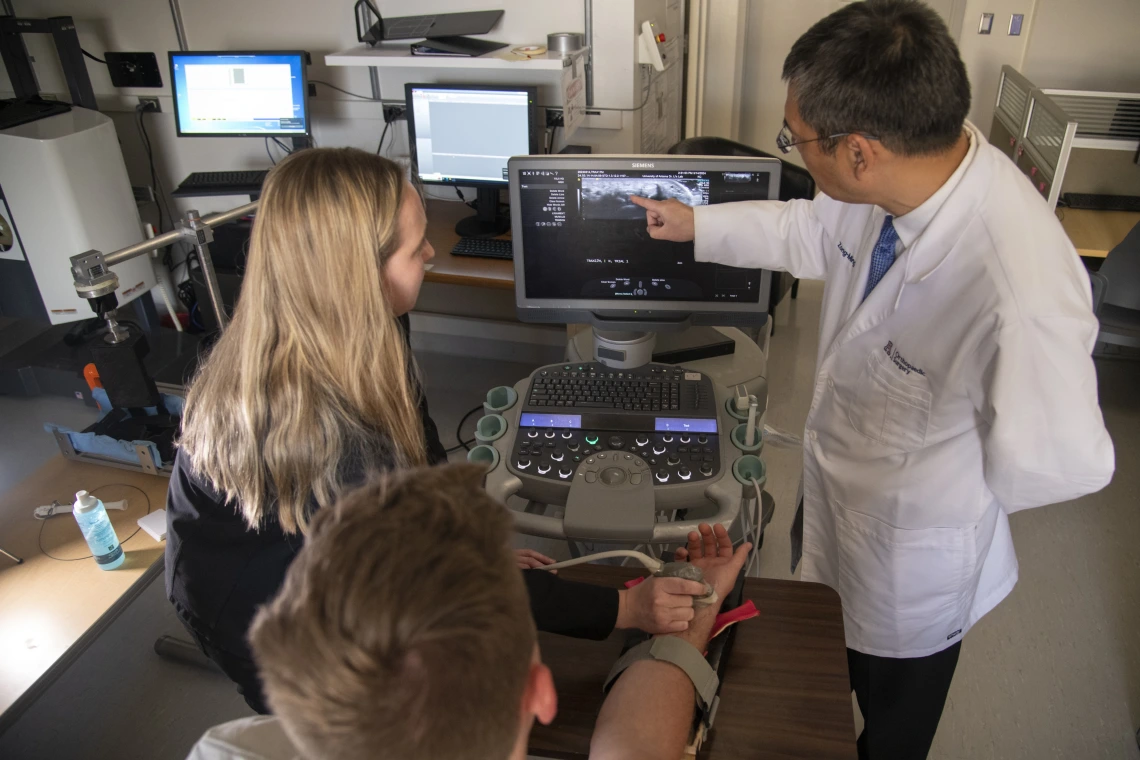
Carpal tunnel syndrome (CTS) is a prevalent hand disorder caused by compression of the median nerve at the wrist. It has an immense impact on national health care, worker productivity, and quality of life. CTS is commonly treated by a surgery that transects the transverse carpal ligament to decompress the median nerve. Our search for a non-surgical CTS treatment alternative has resulted in a novel mechanism of median nerve decompression by applying transverse compression to the wrist to reshape and enlarge the tunnel space. In this project, we design and develop a strategy of carpal tunnel manipulation that achieves treatment efficacy for CTS. Our central hypothesis is that our approach of biomechanical manipulation increases carpal tunnel area, thereby decompressing the median nerve and alleviating CTS symptoms. This project combines basic science and clinical translation, elucidating the underlying morphological and physiological mechanisms of the biomechanical intervention for a systematic and rigorous development of an evidence-based strategy for CTS treatment.

Collagenolysis of the Transverse Carpal Ligament
During carpal tunnel release surgery, the transverse carpal ligament (TCL) is transected to decompress the median nerve. However, transecting the TCL reduces grip strength, causes pillar pain, results in greater carpal bone motion, and may damage the surrounding nerves, vessels or tendons. We aim at developing a novel non-operative treatment for carpal tunnel syndrome by enzymatically degrading the TCL. The objective is to inject collagenase into the TCL and evaluate its enzymatic effect on TCL morphology and mechanics using state-of-the-art robotic and ultrasound technologies. Our hypothesis is that collagenase effectively degrades the TCL, leading to decreased TCL thickness and stiffness in vitro as well as increased TCL length and arch area in situ. The knowledge obtained from this project will guide future in situ carpal tunnel studies, in vivo animal studies, and clinical trials, tapping into the potential of collagenase injection as a novel non-operative treatment for CTS.
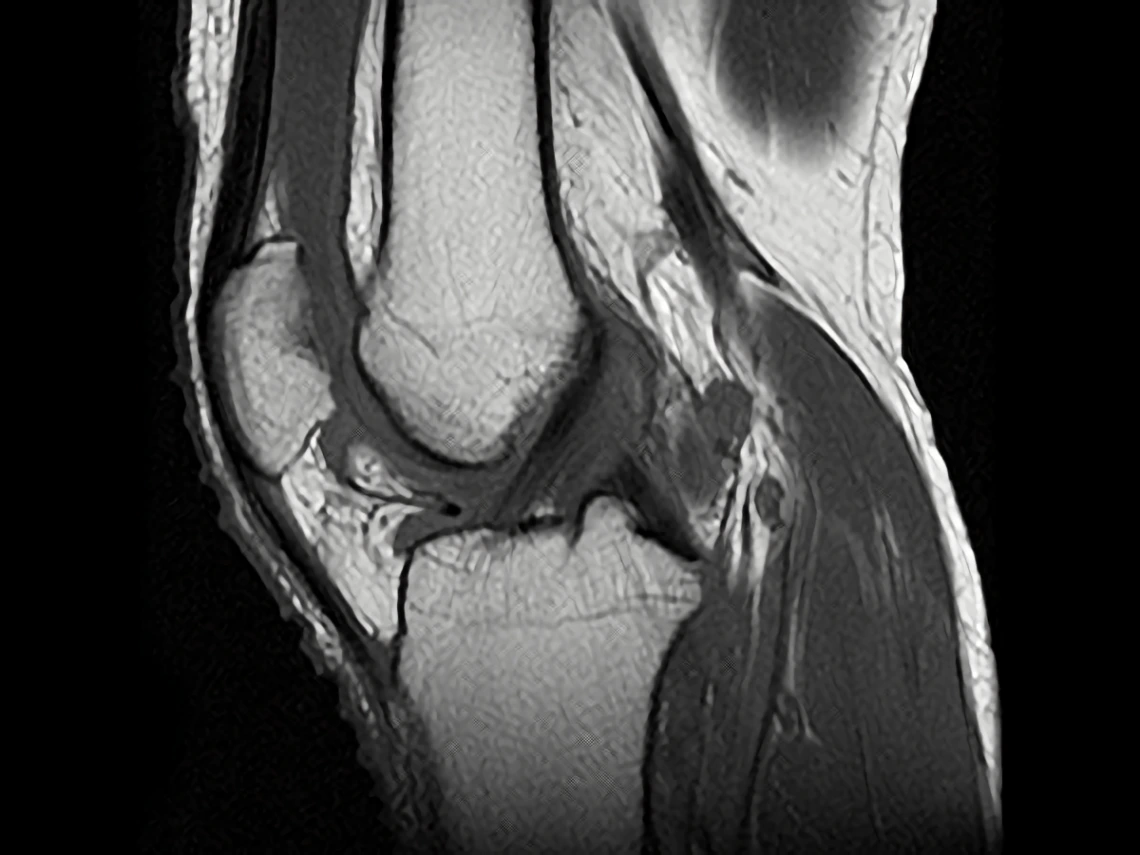
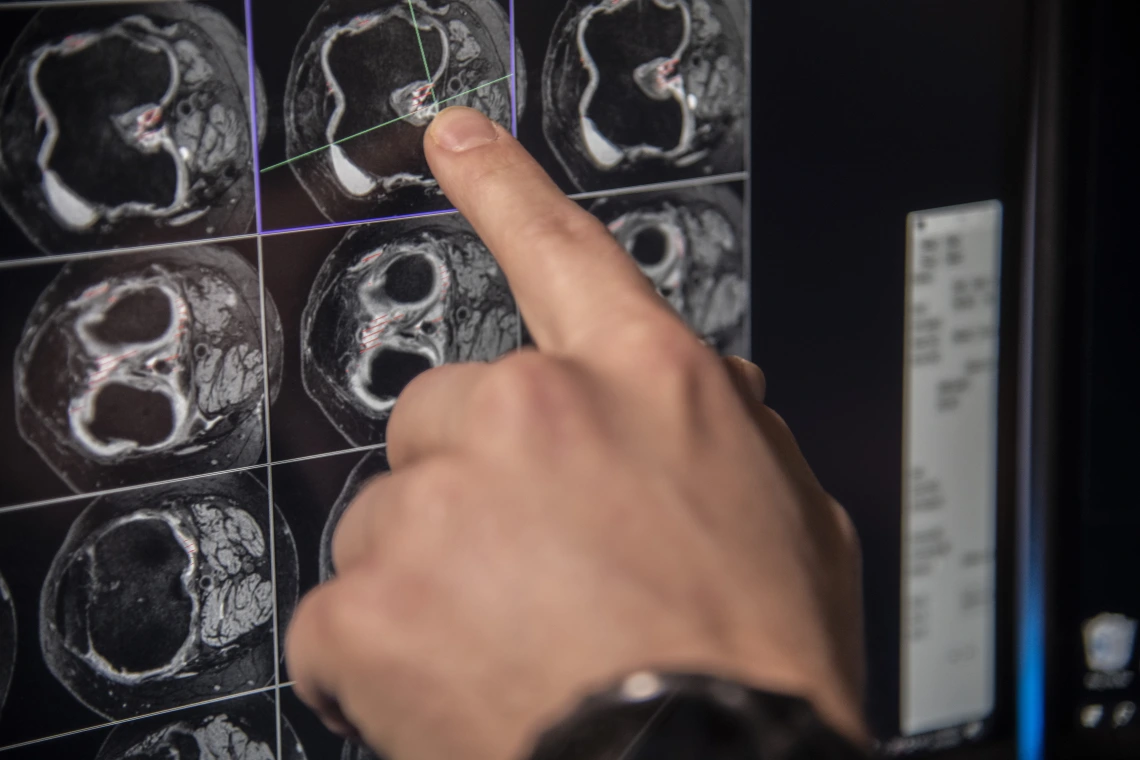
Long Term Significance of Pre-Radiographic Lesions in Persons at Risk for Knee Osteoarthritis
A major barrier to development of disease-modifying therapy for knee osteoarthritis (OA) is the nature of disease progression, a downward spiral involving many tissues. The potential for changing disease course may be highest before this process is in motion. The literature documents cartilage, bone, and meniscal lesions by MRI in knees of some older individuals without radiographic OA, but doesn’t reveal whether they represent early OA. This study seeks to identify an earlier disease onset window; enable future identification of risk factors for clinically important early lesions and prevention strategies that could be introduced earlier in the lifespan; and identify which lesions represent early disease and potential targets of disease-modifying intervention at a point when success may be more realizable.

Orthopaedic Research - Long Bone Growth and Regeneration
Long bone injuries caused during combat or by serious car accidents never heal well. This also applies to surgical removal of large segments of bone due to bone cancer. Currently the first treatment of choice is often use of bone harvested from dead human donors. That dead bone provides support during healing but breaks down over time and fails. The next step is generally complete amputation of the limb. Dr. David Margolis and his team have developed a novel solution that is showing success. A CT scan is collected from the healthy leg and used to 3D print a replica of the bone parts that have been severely damaged. The 3D printed scaffold is filled with stem cells collected from fat tissue taken from the person who was injured. This cell filled construct is placed into the site after the pieces of damaged bone are removed. It guides the growth of new living bone to fill the space. This living bone is strong and vibrant and will last as long as the patient does not get another injury at that location.
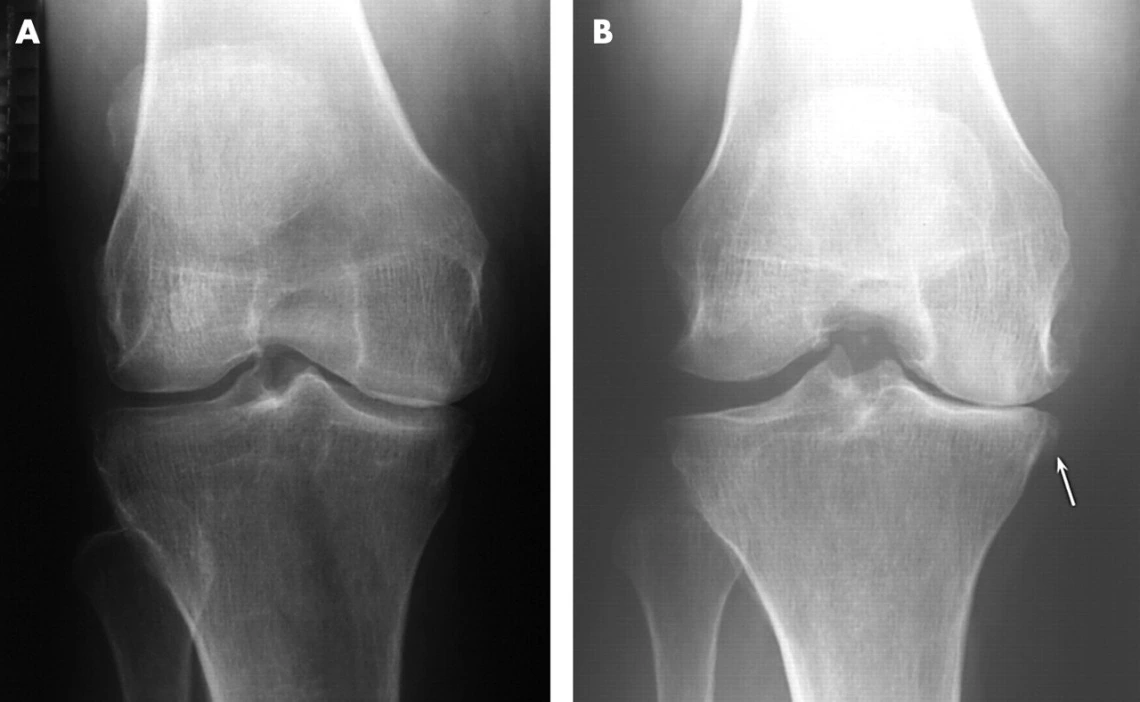
Predictive Performance of Radiographic, MRI and Clinical Symptoms for Subsequent Knee Replacement
The knee is one of the joints most commonly affected by osteoarthritis. Symptoms include pain, stiffness, a grating or grinding sensation when you move the joint and swellings. Treatment depends on how severe the patient’s pain is and ranges from simple painkillers to joint replacement surgery. With more than 600,000 procedures performed each year, the average U.S. cost of a total knee replacement is nearly $50,000. The overall objective of this study is to evaluate the predictive performance of radiographic joint space width, quantitative and semi-quantitative MRI measures and clinical symptoms for subsequent knee replacement.
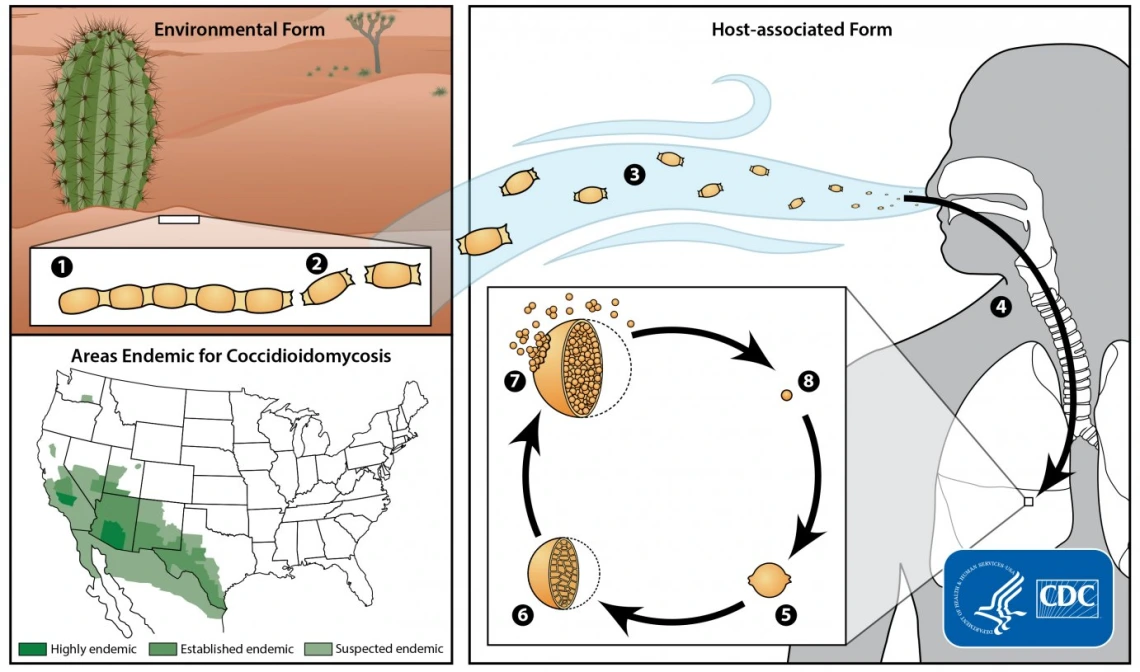
Rheumatoid Arthritis Management in Valley Fever Patients
In the U.S. Southwest, Coccidioidomycosis (cocci) or Valley fever is an endemic fungal infection. It typically presents as a self-limited pulmonary illness. Patients with autoimmune diseases who are on disease-modifying anti-rheumatic drugs (DMARDs) or biologic response modifiers (BRMs) are at higher risk of more severe infection or infection disseminated outside the thoracic cavity. Currently, there are no management guidelines for cocci in such patients.


